Blog
The Pain of Plantar Fasciitis
 Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes. It occurs when this tissue is overstretched or overused, often due to excessive running, standing for long periods, or wearing inadequate footwear. The condition manifests as a sharp, stabbing pain in the heel, particularly noticeable with the first steps in the morning or after long periods of inactivity. Those at higher risk include runners, individuals with high arches or flat feet, people who are overweight, and people who wear shoes with poor arch support. Preventing plantar fasciitis involves wearing supportive footwear, maintaining a healthy weight, and incorporating stretching exercises into daily routines to improve flexibility. Treatment options include rest and stretching exercises, For persistent pain, custom orthotics may be necessary. If you have continued heel pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes. It occurs when this tissue is overstretched or overused, often due to excessive running, standing for long periods, or wearing inadequate footwear. The condition manifests as a sharp, stabbing pain in the heel, particularly noticeable with the first steps in the morning or after long periods of inactivity. Those at higher risk include runners, individuals with high arches or flat feet, people who are overweight, and people who wear shoes with poor arch support. Preventing plantar fasciitis involves wearing supportive footwear, maintaining a healthy weight, and incorporating stretching exercises into daily routines to improve flexibility. Treatment options include rest and stretching exercises, For persistent pain, custom orthotics may be necessary. If you have continued heel pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Gary Saphire, DPM from Parkway Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes and Definition of Heel Spurs
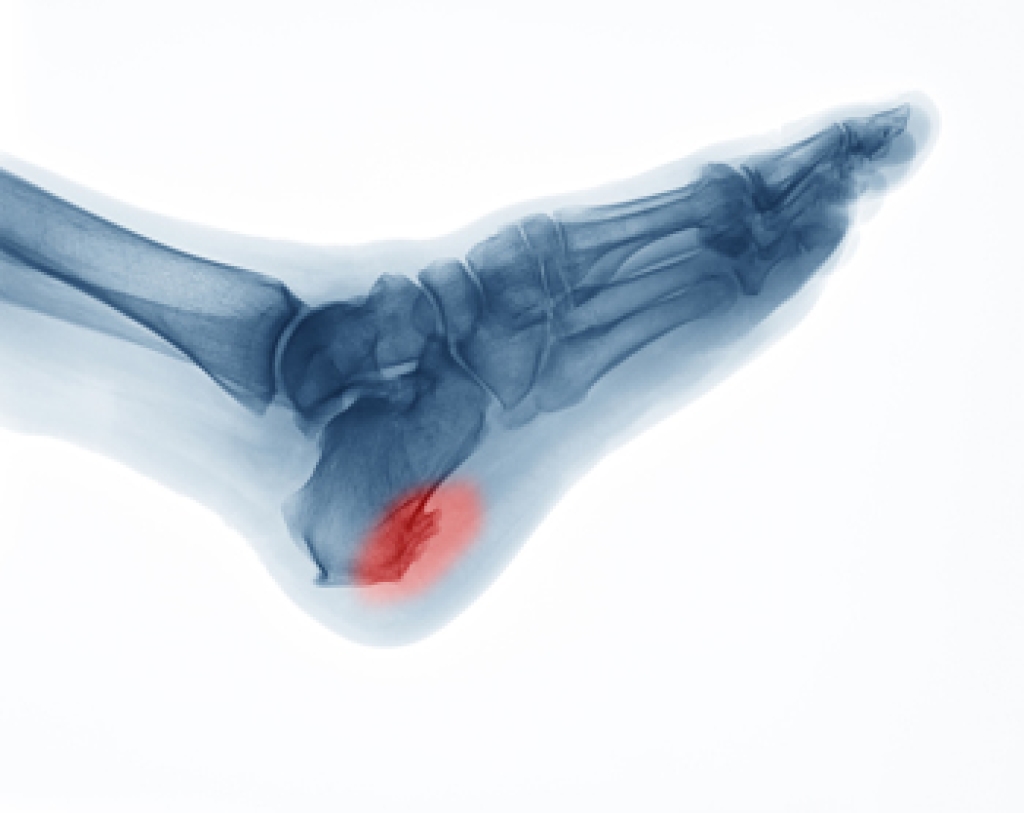 A heel spur, medically known as a calcaneal spur, is a bony growth that develops on the underside of the heel bone. This condition often results from long-term strain on the foot muscles and ligaments, commonly associated with repetitive activities such as running or jumping. Over time, this strain leads to the accumulation of calcium deposits, forming the bony protrusion. Heel spurs are frequently linked to plantar fasciitis, an inflammation of the plantar fascia tissue that runs along the bottom of the foot. Factors contributing to heel spur development include wearing ill-fitting shoes, excessive weight, and having flat feet or high arches. If you have heel pain, it may be indicative of a heel spur, and it is suggested that you consult a podiatrist who can accurately diagnose and offer a comprehensive treatment plan for heel spurs.
A heel spur, medically known as a calcaneal spur, is a bony growth that develops on the underside of the heel bone. This condition often results from long-term strain on the foot muscles and ligaments, commonly associated with repetitive activities such as running or jumping. Over time, this strain leads to the accumulation of calcium deposits, forming the bony protrusion. Heel spurs are frequently linked to plantar fasciitis, an inflammation of the plantar fascia tissue that runs along the bottom of the foot. Factors contributing to heel spur development include wearing ill-fitting shoes, excessive weight, and having flat feet or high arches. If you have heel pain, it may be indicative of a heel spur, and it is suggested that you consult a podiatrist who can accurately diagnose and offer a comprehensive treatment plan for heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Gary Saphire, DPM from Parkway Podiatry. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions, please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Common Running Injuries and Treatment
 Common running injuries include shin splints, Achilles tendinitis, plantar fasciitis, and stress fractures. Shin splints cause pain along the shin bone due to overuse or wearing improper footwear. Achilles tendinitis involves inflammation of the Achilles tendon, while plantar fasciitis affects the band of tissue that connects the heel to the toes, causing heel pain. Stress fractures are tiny cracks in bones due to repetitive force. Evaluation involves a physical examination, imaging tests like X-rays or MRI scans, and a review of the runner's history and habits. Prevention includes proper warm-ups, wearing appropriate shoes, gradually increasing running intensity, and incorporating strength and flexibility training. Treatment varies but often includes rest, compression, elevation, gentle stretching, and sometimes anti-inflammatory medications or orthotics. If you are a runner who has sustained an injury to your feet or ankles, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Common running injuries include shin splints, Achilles tendinitis, plantar fasciitis, and stress fractures. Shin splints cause pain along the shin bone due to overuse or wearing improper footwear. Achilles tendinitis involves inflammation of the Achilles tendon, while plantar fasciitis affects the band of tissue that connects the heel to the toes, causing heel pain. Stress fractures are tiny cracks in bones due to repetitive force. Evaluation involves a physical examination, imaging tests like X-rays or MRI scans, and a review of the runner's history and habits. Prevention includes proper warm-ups, wearing appropriate shoes, gradually increasing running intensity, and incorporating strength and flexibility training. Treatment varies but often includes rest, compression, elevation, gentle stretching, and sometimes anti-inflammatory medications or orthotics. If you are a runner who has sustained an injury to your feet or ankles, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Ankle and foot injuries are common among athletes and in many sports. They can be caused by several problems and may be potentially serious. If you are feeling pain or think you were injured in a sporting event or when exercising, consult with Gary Saphire, DPM from Parkway Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries
The most common injuries that occur in sporting activities include:
- Achilles Tendonitis
- Achilles Tendon Rupture
- Ankle Sprains
- Broken Foot
- Plantar Fasciitis
- Stress Fractures
- Turf Toe
Symptoms
Symptoms vary depending upon the injury and in some cases, there may be no symptoms at all. However, in most cases, some form of symptom is experienced. Pain, aching, burning, bruising, tenderness, tightness or stiffness, sensation loss, difficulty moving, and swelling are the most common symptoms.
Treatment
Just as symptoms vary depending upon the injury, so do treatment options. A common treatment method is known as the RICE method. This method involves rest, applying ice, compression and elevating the afflicted foot or ankle. If the injury appears to be more serious, surgery might be required, such as arthroscopic or reconstructive surgery. Lastly, rehabilitation or therapy might be needed to gain full functionality in the afflicted area. Any discomfort experienced by an athlete must be evaluated by a licensed, reputable medical professional.
If you have any questions please contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Mobility Threats and Risk Factors of Cracked Heels
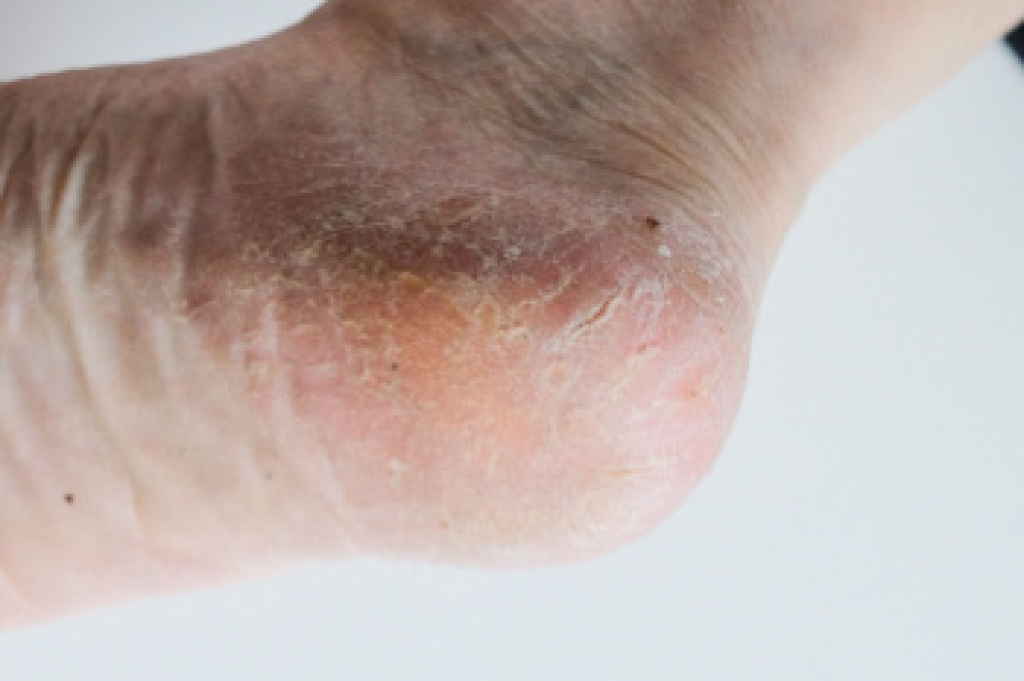
Cracked heels, also known as heel fissures, are a common foot condition where the skin on the heels becomes dry, thick, and cracked. These fissures can range from superficial to deep, causing pain and discomfort, and in severe cases, bleeding and infection. Cracked heels can significantly threaten mobility, making walking or standing painful and challenging. Risk factors include prolonged standing, obesity, wearing open-back shoes, and having dry skin or certain medical conditions such as diabetes and hypothyroidism. Additionally, aging can reduce skin elasticity, increasing the likelihood of developing cracked heels. Maintaining proper foot hygiene, moisturizing regularly, and wearing supportive footwear can help prevent and manage this condition, ensuring that mobility is not compromised and the risk of complications is minimized.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Gary Saphire, DPM from Parkway Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Achilles Tendon Injuries and Treatment
 Achilles tendon injuries often occur due to overuse, sudden increases in physical activity, or inadequate warm-ups before exercise. This tendon, connecting the calf muscles to the heel bone, endures significant stress, especially during activities like running, jumping, or abrupt changes in direction. Such strain can lead to inflammation, known as tendinitis, or even a partial or complete tear. When an Achilles tendon injury happens, individuals typically experience sharp pain or a snapping sensation in the back of the ankle, followed by swelling and difficulty walking. The pain may worsen with activity and improve with rest but can become chronic if untreated. Treatment includes rest and anti-inflammatory medications to reduce pain and swelling. Exercises can help strengthen the tendon and restore flexibility. In severe cases, immobilization or surgery might be necessary. To prevent these injuries, it is important to engage in proper warm-ups, gradually increase activity levels, and wear supportive footwear. If you have Achilles tendon pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and tailored treatment plan.
Achilles tendon injuries often occur due to overuse, sudden increases in physical activity, or inadequate warm-ups before exercise. This tendon, connecting the calf muscles to the heel bone, endures significant stress, especially during activities like running, jumping, or abrupt changes in direction. Such strain can lead to inflammation, known as tendinitis, or even a partial or complete tear. When an Achilles tendon injury happens, individuals typically experience sharp pain or a snapping sensation in the back of the ankle, followed by swelling and difficulty walking. The pain may worsen with activity and improve with rest but can become chronic if untreated. Treatment includes rest and anti-inflammatory medications to reduce pain and swelling. Exercises can help strengthen the tendon and restore flexibility. In severe cases, immobilization or surgery might be necessary. To prevent these injuries, it is important to engage in proper warm-ups, gradually increase activity levels, and wear supportive footwear. If you have Achilles tendon pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and tailored treatment plan.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Gary Saphire, DPM of Parkway Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Types of Neuropathy and Its Impact on Feet

Peripheral neuropathy is a condition caused by damage to the peripheral nerves, often resulting in numbness, tingling, burning sensations, and pain in the extremities. There are several types of peripheral neuropathy, each with its own set of causes and symptoms. Regardless of the underlying cause, peripheral neuropathy can have a significant impact on the feet, leading to decreased sensation, balance issues, and an increased risk of foot injuries and ulcers. Diabetic neuropathy is one of the most common types and is caused by nerve damage from prolonged exposure to high blood sugar levels in people with diabetes. Other types include compressive neuropathy, which occurs when nerves are compressed or pinched, and toxic neuropathy, which can result from exposure to certain medications, chemicals, or toxins. Proper foot care, including regular inspections, supportive footwear, and maintaining good blood sugar levels for diabetes, is essential for managing symptoms and preventing complications associated with peripheral neuropathy. If your feet are affected with any of the above symptoms, it is strongly suggested that you meet with a podiatrist who can offer you effective methods to manage the type of neuropathy you have.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Gary Saphire, DPM from Parkway Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Treatment Options for Bunions
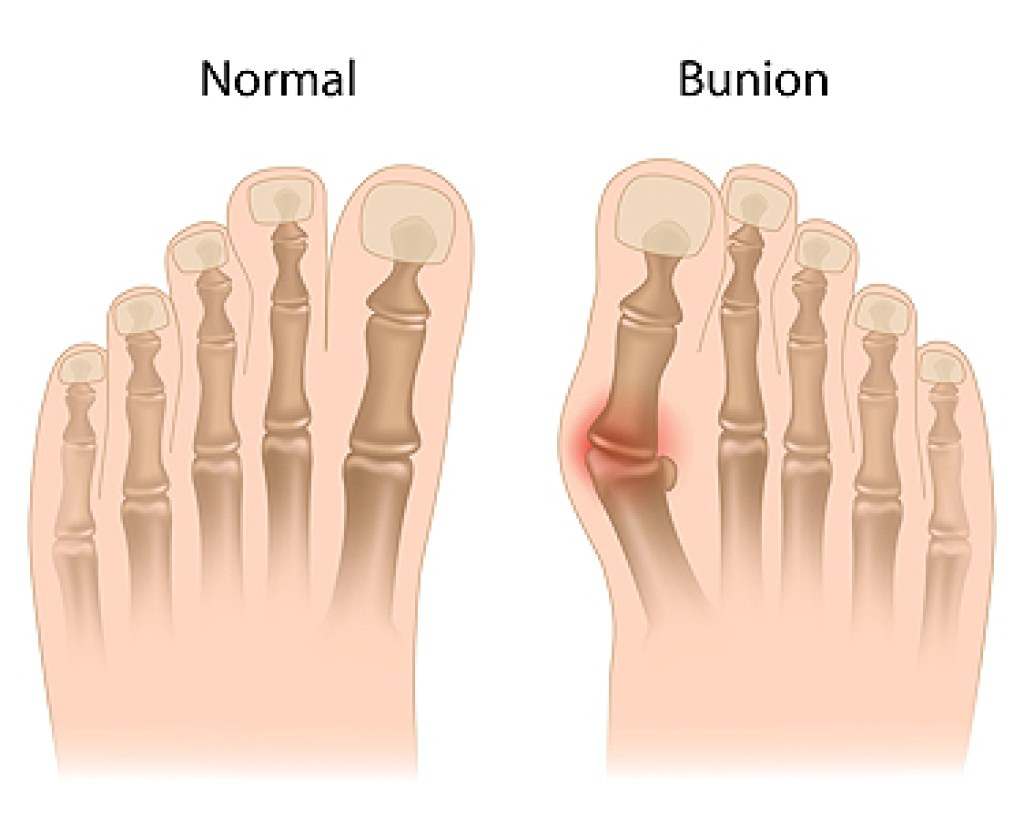
Bunions, medically termed hallux valgus, are a foot deformity characterized by a bony bump at the base of the big toe, while the top of the toe shifts toward the others. Bunions are often accompanied by inflammation and pain. Factors like hereditary predisposition and wearing tight or improper footwear can worsen the deformity. Treatment strategies for bunions typically encompass both non-surgical and surgical approaches. Non-surgical intervention focuses on symptom management and includes wearing well-fitted shoes that provide ample space for the toes. Wearing bunion pads, toe spacers, or orthotic devices for support are among the less invasive treatment options. However, if conservative measures fail to provide relief or if the bunion is severe, surgery may be necessary. Bunion surgery aims to realign the toe joint, alleviate pain, and improve foot function. Surgical techniques include joint trimming and total joint replacement, depending on the severity of the bunion. If you have a bunion that is affecting your daily activities, it's suggested that you schedule an appointment with a podiatrist for a thorough exam and suggested treatment measures.
If you are suffering from bunion pain, contact Gary Saphire, DPM of Parkway Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The Power of Running Is Enhanced by Wearing Proper Footwear

Running offers a multitude of benefits for both physical and mental well-being. It strengthens the cardiovascular system, improves lung function, and boosts metabolism, aiding in weight management and overall health. Beyond the physical advantages, running also promotes mental clarity, stress relief, and a sense of accomplishment. However, to reap these benefits safely and effectively, investing in good running shoes is vital. Quality footwear provides essential support, cushioning, and stability, reducing the risk of injuries such as sprains, strains, and stress fractures. Proper running shoes are designed to accommodate the unique biomechanics of each individual, offering optimal shock absorption and alignment for a smoother, more comfortable stride. By selecting the right shoes for their foot type and running style, runners can enhance performance, minimize discomfort, and prolong their running journey, ensuring they can continue to enjoy the myriad benefits that running has to offer for years to come. Injuries to the foot and ankle can happen from running, and it is essential the right running shoes are chosen. It is suggested that you contact a podiatrist who can treat foot and ankle injuries, and guide you on what the best type of running shoes are right for you.
If you are a runner, wearing the right running shoe is essential. For more information, contact Gary Saphire, DPM from Parkway Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Choosing the Right Running Shoe for Your Foot Type
To increase performance and avoid the risk of injury, it is important to choose the right running shoe based on your foot type. The general design of running shoes revolves around pronation, which is how the ankle rolls from outside to inside when the foot strikes the ground.
- Neutral runners are able to choose from a wide variety of shoes, including minimalist shoes or even going barefoot.
- Runners who overpronate, or experience an over-abundance of ankle rolling, should choose shoes that provide extra motion control and stability.
- Runners who underpronate, or supinate, have feet that have high arches and lack flexibility, preventing shock absorption. They require shoes with more flexibility and cushion.
If you have any questions, please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.